.
Colonoscopy is a simple day-stay procedure performed under sedation. It involves the passage of a flexible tube (colonoscope) about the thickness of a pen into the colon (also called the ‘large intestine’) via the back passage (anus) to allow for careful examination of the entire colon.

When is colonoscopy indicated?
Colonoscopy is performed to diagnose or treat a number of conditions of the colon, including altered bowel habit, constipation, rectal bleeding, or a positive faecal occult blood test (FOBT). It is also indicated in those with a family history of colorectal cancer, or previous polyps.
As well as giving better images than x-ray (barium enema or CT) of what the colon looks like from the inside, colonoscopy also allows for the removal of polyps (polypectomy) or biopsies of the colon. This is a painless procedure done while sedated that avoids the need for major surgery and protects against cancer.
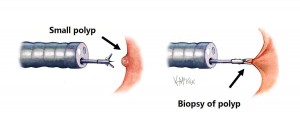
For polyps larger than 5mm, polypectomy is performed by passing a wire loop through the colonoscope and snaring the base of the polyp, which is then electrocauterised with the polyp then retrieved (Figure 3). This process is painless to the patient.

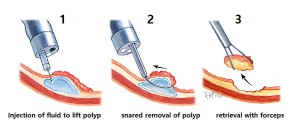
Endoscopic surgery includes techniques such as endoscopic mucosal resection (EMR) or endoscopic submucosal dissection (ESD) which are often needed for Polyps larger than 1.5cm. (Figure 4.)
Why perform a polypectomy?
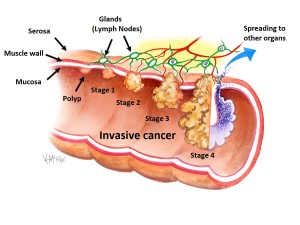
Colorectal cancer is the second largest cancer cause of death in Australia. Polyps are precursor lesions than can become cancer if not removed (Figure 5).
What should I do before my colonoscopy?
Diet restrictions and clear fluids
You will need an empty colon for your colonoscopy. For 24 hours prior to your colonoscopy you can only drink clear fluids (no solid food). Clear fluids are fluids that can be poured through a sieve (no particulate matter) and can be seen through when placed in a glass. Clear fluids include broth or soup, apple juice, lemonade, jelly, and dilute green, orange or black tea or coffee and sports drinks such as Gatorade®, Lucozade® or Gastrolyte®. Ideally at least 3-4 litres of clear fluid should be drunk the day before your colonoscopy.
Bowel Prep
PicoPrep® and Prep KitC are both 3-part laxatives taken orally the day before your colonoscopy and are available at most chemists without the need for a prescription. It is sold as a box of three sachets of white powder that are each mixed as a drink with water. Those having a morning colonoscopy drink their three sachets or bowel prep at 2pm, 4pm and 6pm the day before their colonoscopy. Those having an afternoon colonoscopy drink their three sachets of bowel prep at 6pm and 8pm (day before) and 6am (day of) their colonoscopy. (see Table 1).
| Morning Colonoscopy | Afternoon Colonoscopy | |
| Last Solid Food | Breakfast (Day Before) | Lunch (Day Before) |
| Commence Clear Fluids (i.e. no solid food) | 8am (Day Before) | 1pm (Day Before) |
| 1st sachet of prep | 2pm (Day Before) | 6pm (Day Before) |
| 2nd sachet of prep | 4pm (Day Before) | 8pm (Day Before) |
| 3rd sachet of prep | 6pm (Day Before) | 6am (Day of) |
| Fasting Time (No liquids or solids) | 12Midnight (Day Before) | 7am (Day of) |
| Call & SMS to instruct start time | After 10am (Day Before) | After 10am (Day Before) |
| Present to Hospital | 1 hour prior to start time | 1 hour prior to start time |
| Discharge (Pick-Up) | 3-4 hours after start | 3-4 hours after start |
Table 1. Checklist for patients having colonoscopy.
When should I fast from?
You should fast (no liquids or solids) 6 hours prior to your procedure. If a morning procedure, then fast (no liquids or solids) from midnight the day before, and if an afternoon procedure fast (no liquids or solids) from 7am.
What medications should I stop before my colonoscopy?
If you are taking medications to thin your blood such as aspirin (Dispro®, Astrix®, Cartia® Cardiprin® Solprin® Asasantin®) clopidogrel (Iscover® or Plavix®), warfarin (Coumadin® or Marevan®) or rivaroxaban (Xarelto®) dabigatran (Pradaxa®) you should speak with your surgeon about the indication for these. Sometimes it is necessary to stop blood-thinning medications 7 days prior to your colonoscopy to reduce the risk of bleeding following polypectomy.
Diabetic medications should not be taken the morning of your surgery or procedure to avoid hypoglycaemia (i.e. low blood sugar). Diabetic medications include Insulin (Humalog®, Humulin®, UltraLente®, Lantis®, Lente®, Levemir®, Mixtard®, NovoLog, NovaMix, Novolin®) diamicron (Gliclazide®, Daonil®) and metformin (Glucophage®, Glumetza®, Glocomet®, Riomet®).
When to present to hospital?
You need to present to hospital 1 hour prior to your colonoscopy. You will be instructed by phone and text message after 10am the day before your procedure of your planned start time.
What happens before and after colonoscopy?
A nurse will direct you to the endoscopy unit. You will remove your clothes and underwear and wear a hospital gown. You will meet your surgeon and anaesthetist before your procedure to discuss any questions you may have. Colonoscopy will be performed with intravenous sedation. Colonoscopy may take from 30 to 60 minutes depending on whether or not biopsies are taken or polyps removed. You will then spend 1 hour in recovery until the effects of sedation have worn off. It is common to experience some abdominal cramping until you have passed much of the inflated air. Then you will spend 1 hour in the discharge lounge and be given a small meal and will meet with your surgeon to discuss your results before being allowed to have a friend or relative drive you home approximately 3 hours after your procedure start time.
When will I be ready for discharge home?
You will be ready for discharge home approximately 3 hours after the planned start time for your colonoscopy.
How do I get home from hospital?
If your procedure is being done as a day-stay procedure you will need to have someone drive you home, as you are unsafe to drive a car immediately after an anaesthetic. Some hospitals will allow a taxi home, however it is preferable that you travel with a friend or relative.
Biopsy results and follow-up appointments
You need to call 1300 265 666 after 1 week to obtain any biopsy results or to make a follow-up appointment. If you have had polyps removed or have a family history of bowel cancer, you will be entered into a recall database for a reminder phone call for a repeat colonoscopy every 3-5 years depending on your circumstances.
What are the risks of colonoscopy or polypectomy?
Colonoscopy and polypectomy are very safe with very small risk of complications, although complications can occasionally occur. Anaesthetic complications are uncommon. Pain or swelling of the arm vein may occur at the site of injection of your anaesthetic. This will eventually disappear. Perforation of the colon is a rare but severe complication where a hole is made in the bowel. It occurs in less than 0.08% of cases[1]. The risk of perforation following colonoscopy where a polypectomy is also performed is 0.3-1.0%. If this happens, and the hole is small, it may settle with antibiotics, however in some cases it requires abdominal surgery to close the defect in the bowel wall. Care will be taken to avoid this complication.
If you would like to have a gastroscopy performed as well as colonoscopy under the one anaesthetic, please request this from your surgeon.
References
- Arora G, et al, Risk of perforation from a colonoscopy in adults: a large population-based study. Gastrointest Endosc. 2009.