A cholecystectomy is surgery to remove the gallbladder. It is usually done using a keyhole (laparoscopic) approach where a tiny video camera and surgical equipment are inserted through 4 small cuts in the abdomen.
Why is the procedure performed?
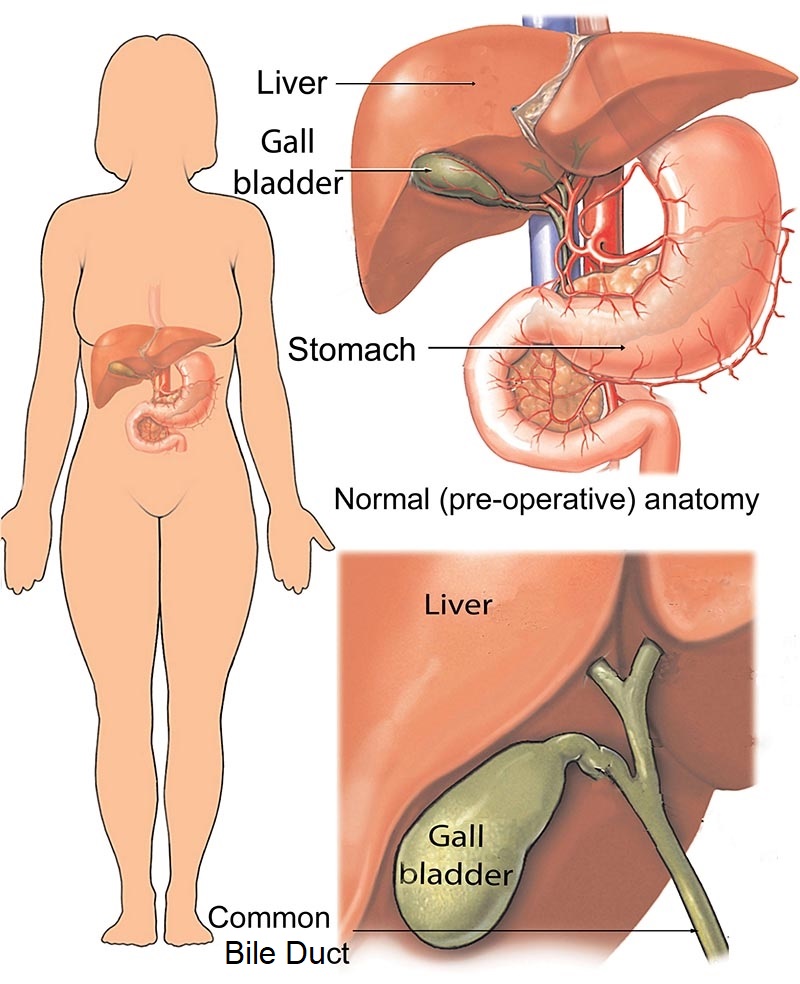
The gallbladder is a small organ that sits just below the liver on the right side of your abdomen. It collects and stores bile from your liver, which is used by the gut to help digest food.
Sometimes the gallbladder becomes blocked with gallstones that form within the bile and can cause pain, bloating, nausea and vomiting. Other complications can also occur, including inflammation of the gallbladder, inflammation of the pancreas, jaundice and infection.
Cholecystectomy is performed under general anaesthetic.
Sometimes, gallstones, particularly if very small, can move from the gallbladder into your Common Bile Duct (CBD). Bile ducts are ‘pipes’ that carry bile from the liver to the gallbladder and from the gallbladder to the small intestine. The CBD is the Common Bile Duct shared by both the liver and pancreas.
How to prepare for the procedure
If you need to have a cholecystectomy, you will be asked to be nil by mouth (no food or liquid) for six hours prior to your surgery start time. If you need to take medications, you may have a sip of water.
Your surgeon will discuss with you whether to stop taking any medicines. Make sure you follow all the instructions from your surgeon. Medications that thin your blood and diabetic medication should be discussed with your surgeon, and a plan made about when and if to stop these medications. Most diabetic medications are not taken the day of your surgery, as while fasting there is a risk of having a low blood sugar level. Most blood thinners such anti-platelet agents including aspirin (Cartia®) or Clopidogrel (Plavix®) are stopped a week before surgery if safe to do so. Other Anti-coagulant blood thinners such as Apixiban®, Xeralto®, and Warfarin are stopped 3-4 days before your surgery with subcutaneous (Clexane®) injections (1mg per kg) given daily the two days before your surgery.
Most patients go home the day after surgery, but you may need to stay in hospital longer depending on your condition.
What happens during the procedure
Most cholecystectomies are performed laparoscopically, which means they use a keyhole approach through small incisions. The surgeon will make 4 small cuts (incisions) in your abdomen so they can introduce a piece of equipment known as a laparoscopic telescope through one of the incisions. These are each less than one centimetre. This will allow them to see inside your abdomen.
They will then pass metal tubes through the other incisions. The surgeon will put carbon dioxide inside your abdomen to lift the wall of the abdomen away from the organs. They will then perform an on table x-ray after injecting dye into the cystic duct to confirm correct anatomy, and the absence of any common bile duct stones. This is called an intra-operative cholangiogran. Once this is done, surgical clips are used to close off the cystic ducts and arteries leading to the gallbladder before dividing these. The gallbladder is then removed from the surface of the liver using electrocautery (diathermy) and placed in a sterile bag called and Endocatch® used to remove the gallbladder via the umbilical port. The finial length of the umbilical incision will depend on the largest size of your gallstone.
After the gallbladder has been removed, the carbon dioxide is allowed to escape before the incisions are stitched with dissolvable monocryl sutures. The clips will stay inside you, and are safe for MRI. They will not set of airport security alarms.
If your gallbladder is very inflamed you may need ‘open cholecystectomy’, which requires a larger cut in your upper abdomen usually below the right costal margin. The risk of needing to convert from laparoscopic to open cholecystectomy is less than 1% for a thin walled gallbladder, but for a thickened gallbladder about 5%. For an acutely inflamed gallbladder, about 15%.
What to expect after the procedure
You will be monitored in recovery for some time and once alert transferred to your bed in the surgical ward. Most patients stay overnight and are discharged the following day after review by your surgeon. If you have a drain, this is typically removed before being discharged.
You may have some side effects from the general anaesthetic such as a headache, nausea or vomiting, which can be controlled with medicine.
You will have some pain in your abdomen after the operation, which can be controlled using pain relief. Typically simple Over-the-countersigning pain killers such as paracetomol (Panadol ®), and ibuprofen (Nurofen®) are sufficient. A stronger pain killer tapentadol (Palexia IR®) may be prescribed. This may cause constipation so an over-the-counter stool softener such as Docusate with Sennosides (Coloxyl with Senna®) may be required. You may also have some pain in your shoulder from the gas used in the operation, which can be eased with walking.
You will have a drip in your arm at first, which will be removed after the anaesthetic wears off. You can take sips of water at first then slowly get back to eating and drinking normally. Most people are able to tolerate a light diet the evening of their surgery.
Your wounds will have dissolvable stitches and you may also have a drain in your side to allow fluid to leave your body. This drain is about the thickness of a pen, but is soft and flexible. On the end of the drain is a bag to allow fluid to collect. This drain is usually removed the next day by the nursing staff, and is usually not painful. The drain site is Then covered with a water proof Douderm dressing. All your dressings are water prof. If blood collects underneath your dressing then your nurse can clean your wound and reapply a clean dressing before your discharge home.
You will be tired at first. Do not drive for the first 5 days, smoke or lift heavy weights (greater than 10 kilograms). You can expect to recover fully and return to your normal activities within 2 weeks. A medical certificate for two weeks off work is routinely provide to all patients.
Contact your doctor immediately if you have:
- a lot of discharge from the wounds
- a fever
- pain that can’t be controlled by pain relief medicine
- swelling, tenderness or redness in the abdomen
- yellow eyes or skin
Risks
A cholecystectomy is a very safe procedure. As with all surgery, however, there is a very small risk of complications, which include:
- bile leak (less than 1-4%)
- common bile duct injury (less than 1 in 1000)
- bleeding
- blood clots in your legs
- infection
- injury of other organs such as bowel or liver
- pancreatitis
- complications related to general anaesthetic, including heart attack, allergic reaction (less than 1 in 10,000) and death (less than 1 in 100,000).